Reflex sympathetic dystrophy (RSD) is a nerve disorder that affects pain regulation.
Doctors now refer to RSD as “type 1 complex regional pain syndrome” or “complex regional pain syndrome (CRPS) 1.”
People with RSD feel excessive pain, usually in their limbs or extremities. They may also experience changes in body temperature, unusual sweating, a decreased range of motion, and other symptoms.
This article explores the symptoms and causes of RSD and available treatment options.
RSD, or CRPS 1, is a disorder that disturbs pain regulation in nerves within the central and sympathetic nervous systems.
The central nervous system controls most functions of the brain and body. The sympathetic nervous system is responsible for rapid, involuntary responses to pain or stress.
People with CRPS 1 typically experience pain in the extremities, such as the fingers and toes.
There is a second type of CRPS, called CRPS 2. CRPS 1 occurs in the absence of trauma to the affected nerves. CRPS 2 occurs as a direct result of trauma.
Although the causes of CRPS 1 and CRPS 2 are different, the disorders share characteristics. Doctors, therefore, can have difficulty distinguishing between them.
The two most important features of CRPS 1 are allodynia and hyperalgesia.
Allodynia involves feeling pain from stimuli that are not typically painful. For example, a person with allodynia may experience pain from a light touch. A doctor may test for it by lightly touching a person’s skin with a cotton swab.
Hyperalgesia involves increased sensitivity to painful stimuli. An excessive response to pain could indicate hyperalgesia to a doctor.
People with CRPS 1 may also experience dysfunction of sweat glands and blood vessels. These issues could result in:
- changes in body temperature
- unusual sweating
- changes in skin color
- changes in the growth and survival of cells that regenerate hair, skin, and nails
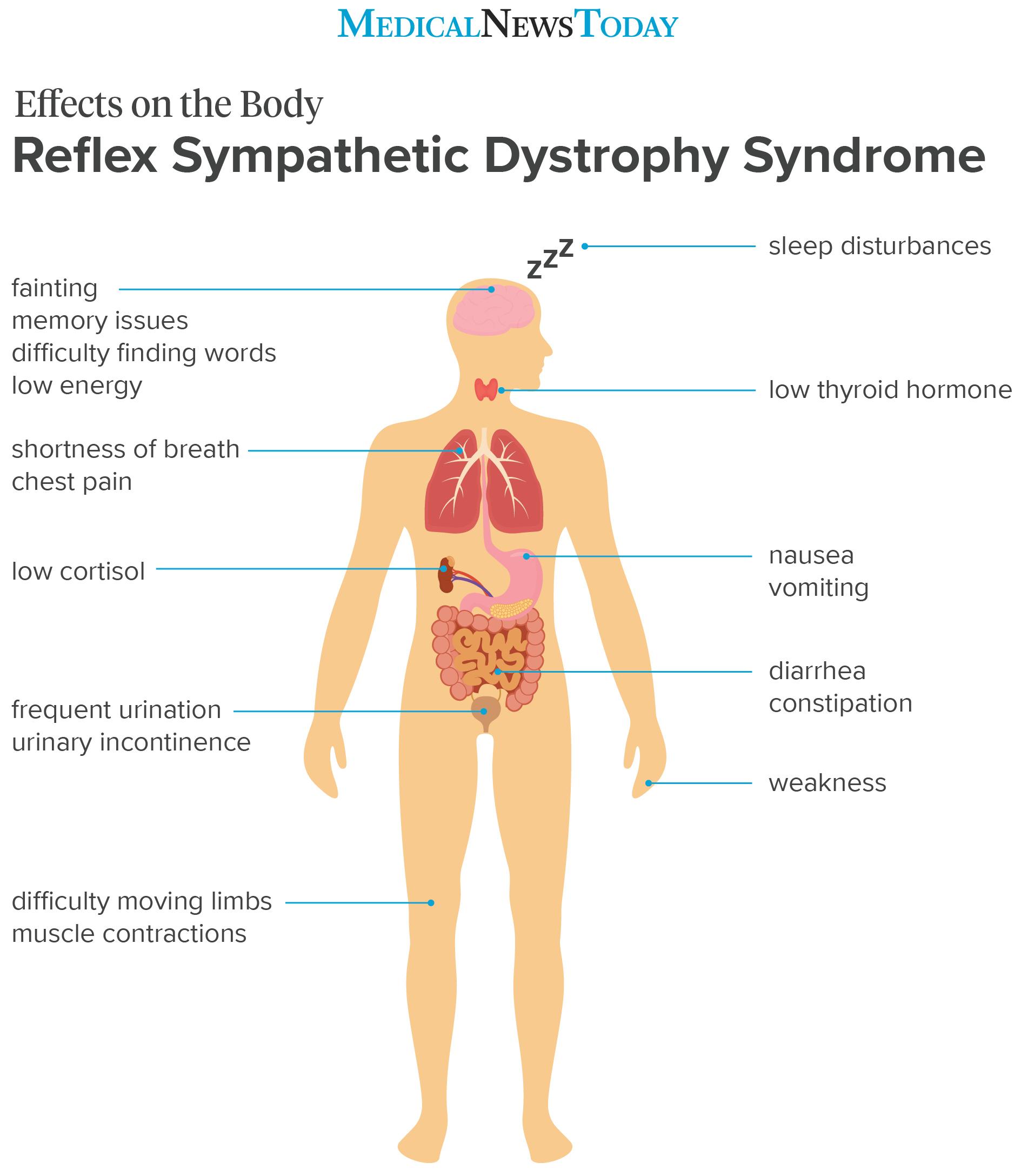
Some people experience widespread, or systemic, effects of CRPS 1. Systemic effects extend to other systems within the body.
The following table shows various systemic effects of CRPS 1 and their associated symptoms.
Diagnosing CRPS 1 can be challenging. This is because it shares many symptoms with other conditions, such as:
Doctors use the Budapest criteria to diagnosis CRPS. In order to meet these criteria, a person must have either allodynia or hyperalgesia, plus at least one symptom in two or more of the following categories:
- Sensory symptoms: These relate to the physical senses. An example is excessive skin sensitivity.
- Vasomotor symptoms: These involve blood vessel constriction or dilation. Examples include unusual body temperature or skin color changes.
- Sudomotor or edema symptoms: Sudomotor symptoms result from stimulated sweat glands. Edema symptoms involve swelling.
- Motor or trophic symptoms: Motor symptoms affect movement, while trophic symptoms involve hormones. These may, for example, affect hair growth.
A doctor will diagnose CRPS if a person meets the above criteria and if their symptoms do not fit those of a different diagnosis.
CRPS often improves on its own. However, it can progress to a chronic pain condition.
Currently, there are no set guidelines for the treatment and management of CRPS 1. However, a team of doctors, physiotherapists, and occupational therapists can work together to design a treatment plan for each individual.
A doctor may recommend treating CRPS 1 with one or more drugs. Some of these drugs may include:
- oral corticosteroids
- anticonvulsant medications, such as gabapentin (Neurontin)
- antidepressants with pain relieving actions, such as duloxetine (Cymbalta)
- the local anesthetic lidocaine
- opioids
In some situations, combining drugs of different classes can improve a person’s symptoms.
Other treatments include:
- oral vitamin C, a supplement that helps fight inflammation-producing free radicals
- topical capsaicin, often a cream or ointment that contains capsaicin, which can help relieve pain naturally
- nerve blocks, local anesthetics that can be injected around the affected nerves
- serial sympathetic ganglion blocks, injected drugs that can block nerve cells within the sympathetic nervous system
- neuromodulation, a procedure that involves using targeted drugs or electrical activity to alter nerve activity
- spinal cord stimulation, a procedure that delivers electrical pulses to the spinal cord to mask pain signals before they reach the brain
- surgical sympathectomy, a procedure that removes the nerve supply to the sweat glands
- cognitive behavioral therapy, a form of psychotherapy that can help treat depression and anxiety, which often occur alongside CRPS
A 2013 report on CRPS 1 treatment concludes that there is insufficient evidence to support the use of one treatment over another. Further high-quality research is necessary to identify the most effective treatments for pain and disability among people with CRPS 1.
Doctors suggest that multiple factors may contribute to the development of CRPS 1. These include:
- abnormal nerve transmission
- an unusually sensitive central nervous system
- dysfunction in the autonomic nervous system, which controls unconscious bodily functions
The causes of these issues may relate to genetics, inflammation, psychological factors, or a combination.
CRPS often improves gradually over time. However, some people with the condition go on to experience chronic pain.
As the 2013 report highlights, further high-quality studies are needed to develop clear treatment guidelines for this syndrome. However, since the incidence of CRPS is low, researchers have difficulty finding suitable study participants.
Anyone who experiences chronic pain should talk to their healthcare provider about treatment options.
RSD, or CRPS 1, is a nerve disorder that primarily causes pain in the limbs and other extremities.
Other symptoms of CRPS 1 include changes in sweating and hair and nail growth, as well as a decreased range of motion in the affected limbs. Some people with the condition also experience digestive, urinary, and cardiorespiratory issues.
Although certain criteria help doctors diagnose CRPS 1, treatment guidelines do not yet exist. A team of healthcare professionals can design a treatment plan based on each individual’s symptoms. This plan may include supplements, medications, and procedures to block nerve pain.
Developing guidelines for the treatment and management of CRPS 1 will require more high-quality research.
Source link
 Black America Breaking News for the African American Community
Black America Breaking News for the African American Community